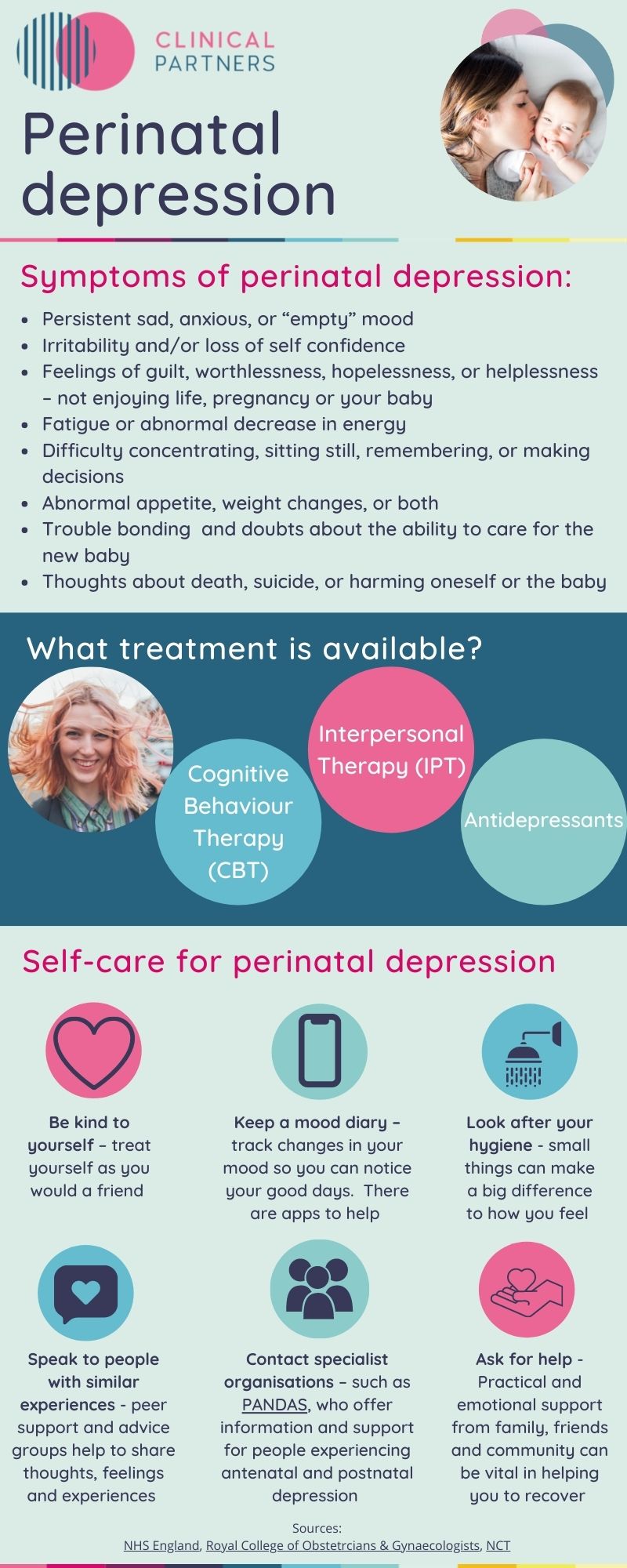
Perinatal depression: symptoms, treatment and self-care tips
Up to two in ten women suffer some type of mental health difficulty in the perinatal period. And with reports showing a decline in maternal mental health since the start of the pandemic, the topic is coming into sharper focus than ever.
Postnatal depression, the type of depression many parents experience after having a baby, is more commonly discussed and widely understood. But it’s perhaps less commonly known that many people experience antenatal depression, which occurs during pregnancy - and some people can experience both.
Perinatal depression, meanwhile, can occur anytime from the start of pregnancy up to a year after giving birth, so covers both the antenatal and postnatal periods.
To help build some basic understanding, we've outlined the typical symptoms, available treatments and listed some self-care tips for people experiencing perinatal depression.
Please be aware that while some of these symptoms are common for parents to experience during and after pregnancy, it's important to mention them to your doctor if you're concerned you might be experiencing perinatal depression.
Rae Britton
Content Editor
BA Joint Hons, QTS
Rae oversees the creation of a range of content that offers insight, support and guidance on mental health issues. She is both passionate and ably qualified. She is a former primary school teacher, while she also has three children, two of whom are neurodivergent, having ADHD and autism. This means she can combine her expertise and direct experience to shape content that helps those in need to survive, thrive and excel.